Matching blood types is a crucial process in transfusions, organ transplants, and genetic testing. One of the most accurate ways to identify and match blood types is through electrophoresis, a technique that separates proteins based on their size, charge, and other properties. This method can identify specific blood group antigens that play a key role in compatibility between blood donors and recipients. The electrophoresis process provides a more detailed view of the blood’s molecular composition, which enhances the accuracy of matching blood types. In this article, we’ll explore how electrophoresis works and why it’s essential in the process of blood type matching.
What Is Electrophoresis?
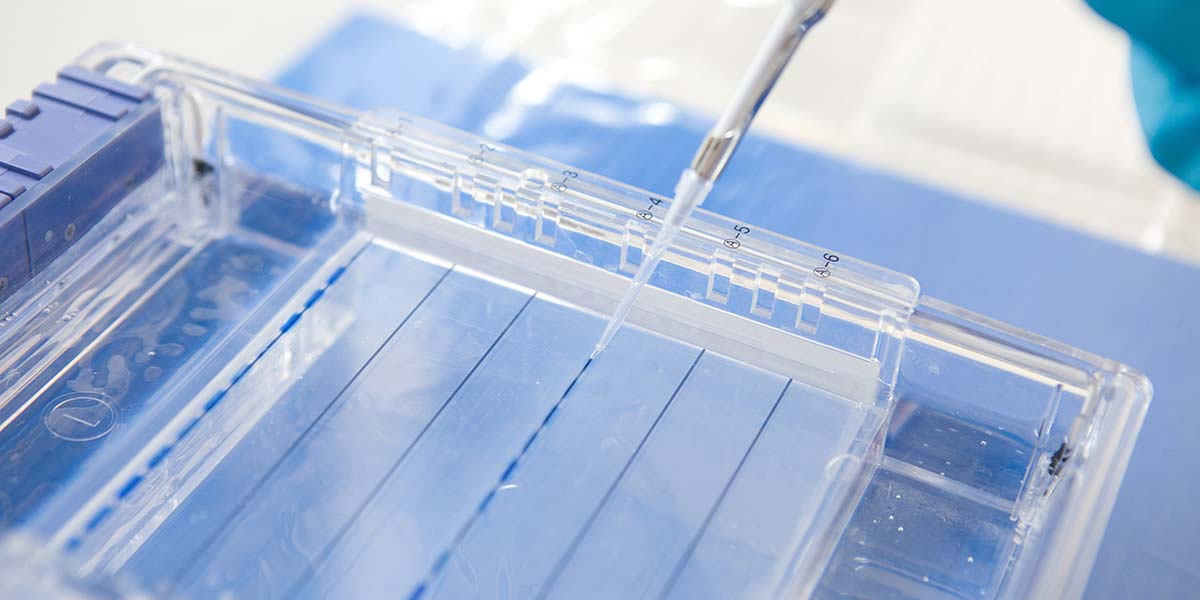
Electrophoresis is a laboratory technique that separates charged molecules, such as proteins or nucleic acids, through a medium like a gel or liquid when an electric field is applied. The process works because charged molecules move at different rates depending on their size and charge, creating a distinct pattern. This pattern helps scientists identify specific proteins or markers that are crucial in blood typing, such as the presence of antigens or antibodies. In blood typing, electrophoresis allows researchers to identify the specific blood group of a sample by analyzing the unique markers present. The ability to precisely determine blood group antigens is vital for safe blood transfusions and transplants.
Blood Typing: Why It Matters
Blood type matching is a critical part of modern medicine, especially in transfusions and organ transplants. The compatibility between the blood of a donor and recipient is essential to avoid serious immune reactions. Mismatched blood can lead to the recipient’s immune system attacking the transfused blood cells, causing potentially life-threatening complications. Electrophoresis helps prevent this by ensuring that blood types are identified with great accuracy. Blood types are determined by the presence or absence of specific proteins called antigens on the surface of red blood cells, which can be detected through electrophoresis.
The Role of Antigens in Blood Type Matching
Blood group antigens, such as the A, B, AB, and O markers, are present on the surface of red blood cells and play a central role in blood typing. The presence or absence of these antigens determines a person’s blood group and compatibility with others. When conducting blood tests using electrophoresis, these antigens can be detected and analyzed. For example, blood with A antigens will react with anti-A antibodies, while blood with B antigens will react with anti-B antibodies. By identifying these antigen-antibody reactions, electrophoresis provides a clear picture of a person’s blood type and its compatibility with potential donors or recipients.
How Electrophoresis Works in Blood Typing
The electrophoresis process in blood typing involves applying a blood sample to a gel or other medium and then applying an electric field. The proteins in the blood move through the medium at different rates based on their charge and size, creating a separation pattern. In blood typing, this pattern reveals the specific antigens and antibodies in the sample, providing a more detailed analysis than traditional blood typing methods. The resulting electrophoretic pattern can show the presence of blood group antigens such as A, B, or Rh factor, which are essential for matching blood types. This method ensures high accuracy in determining blood type compatibility.
Benefits of Using Electrophoresis for Blood Matching
One of the main advantages of using electrophoresis in blood typing is its precision. Traditional methods may miss subtle differences in blood group antigens, which could lead to mismatches in blood transfusions or organ transplants. Electrophoresis, on the other hand, provides a clearer and more accurate identification of blood type. Additionally, this technique can also detect rare blood group antigens that may not be identified by other methods. By ensuring a more accurate match, electrophoresis helps improve the safety and success of medical procedures that involve blood exchanges.
Vote
Who is your all-time favorite president?
Electrophoresis vs. Traditional Blood Typing Methods
Traditional blood typing methods, such as agglutination tests, rely on the reaction between antibodies and blood samples to determine blood types. While effective, these methods can be less sensitive in detecting rare blood types or subtle differences in antigens. Electrophoresis, on the other hand, allows for a more comprehensive analysis of blood group markers. It can identify specific proteins on the surface of red blood cells and even detect minor variations in antigen expression. This increased sensitivity makes electrophoresis a preferred method in many modern laboratories, particularly for complex blood type matching.
Challenges in Electrophoresis for Blood Typing
While electrophoresis is a powerful tool for blood typing, it does come with challenges. For one, the equipment needed for electrophoresis can be expensive, which may limit its accessibility in some settings. Additionally, interpreting electrophoretic patterns requires significant expertise and can be time-consuming. The process also requires a high degree of precision in preparing and running samples, which can lead to human error. Despite these challenges, the benefits of using electrophoresis in blood typing far outweigh the potential drawbacks, especially when it comes to matching rare or complex blood types.
The Future of Electrophoresis in Blood Matching
The future of electrophoresis in blood type matching looks promising, with advancements in technology making the process more accessible and efficient. New automated electrophoresis systems are being developed to reduce human error and improve the speed of results. In addition, research is underway to explore how electrophoresis can be used to detect even more blood group antigens, enhancing the precision of blood matching. As these technologies evolve, electrophoresis could become the gold standard for blood typing in both clinical and research settings. The integration of this technology into routine medical practice could lead to safer and more accurate blood transfusions and organ transplants.
Applications Beyond Blood Typing
While electrophoresis is most commonly associated with blood typing, its applications extend far beyond that. This technique is also used in genetic research, protein analysis, and even the diagnosis of certain diseases. By separating proteins and nucleic acids, electrophoresis can help scientists identify markers for genetic disorders, cancers, and other health conditions. The ability to analyze proteins and other molecules with such precision makes electrophoresis an invaluable tool in many fields of medicine and biology. As research advances, electrophoresis could play a key role in diagnosing and treating a wide range of diseases.
Key Benefits of Electrophoresis for Blood Matching
- Provides accurate and reliable blood typing results.
- Detects rare or complex blood types with precision.
- Improves the safety of blood transfusions and organ transplants.
- Can identify specific blood group antigens beyond the ABO system.
- Enhances the understanding of blood compatibility in complex medical cases.
- Minimizes the risk of mismatched transfusions or organ rejection.
- Helps in genetic and disease research by analyzing blood samples.
Watch Live Sports Now!
Dont miss a single moment of your favorite sports. Tune in to live matches, exclusive coverage, and expert analysis.
Start watching top-tier sports action now!
Watch NowChallenges of Using Electrophoresis for Blood Typing
- Requires specialized equipment and expertise.
- Can be costly for smaller clinics or hospitals.
- Time-consuming sample preparation and analysis.
- Potential for human error in interpreting results.
- Requires regular calibration and maintenance of equipment.
- May not be necessary for routine blood type testing.
- Requires a controlled environment to ensure accurate results.
Pro Tip: While electrophoresis offers high accuracy, it is most beneficial when used in cases where traditional blood typing methods might fail, such as with rare blood types or complex medical cases.
| Factor | Electrophoresis | Traditional Methods |
|---|---|---|
| Accuracy | High, detects rare antigens | Moderate, may miss subtle differences |
| Cost | Higher, requires specialized equipment | Lower, uses basic reagents |
| Time | Longer, requires careful sample preparation | Faster, more straightforward |
“The precision of electrophoresis in blood typing ensures that life-saving blood transfusions and organ transplants are as safe as possible.”
In summary, electrophoresis represents a vital advancement in blood type matching and offers a more detailed and accurate approach to determining blood compatibility. While it does come with challenges, such as high costs and the need for specialized expertise, the benefits far outweigh these drawbacks. As medical science continues to evolve, electrophoresis will likely play a larger role in ensuring the success of blood transfusions, organ transplants, and even in genetic research. For those in the medical and research fields, understanding the power of electrophoresis can help improve outcomes and safety. Bookmark this article to stay informed about this cutting-edge technique and share it with colleagues to keep them up-to-date!